Abstract
Introduction: Acute myeloid leukemia (AML) in the elderly is a therapeutic challenge, and global evaluation of comorbidity, performance status, fitness and frailty is crucial for therapeutic decision of treatment intensity. Accurately predicting risks and benefits of available therapies is particularly difficult, as it relies on subjective criteria, no geriatric scores being validated so far. The aim of this study was to evaluate the impact of a standardized geriatric assessment at diagnosis in a prospective cohort of newly diagnosed AML in elderly patients, and to investigate correlations between geriatric scores and overall survival.
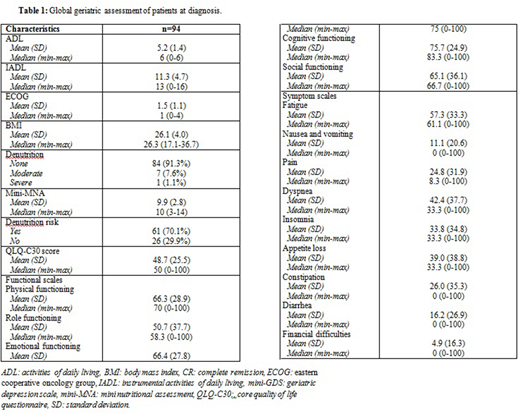
Methods: All patients aged ≥ 70 years with newly diagnosed AML were prospectively included in this cohort. They all benefited from an exhaustive geriatric assessment in addition to standard AML workup, including ADL, IADL, ECOG, comorbidities, nutritional status (assessed by BMI and mini-MNA), cognitive impairment (mini-COG, mini-GDS), quality of life (QLQ-C30), functional scales (physical, role, emotional, cognitive and social functioning), symptom scales (fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, financial difficulties) and frailty criteria (physical activity, energy visual scale, mobility, nutrition). Patients were treated according to international guidelines, with intensive chemotherapy, hypomethylating agents, subcutaneous low-dose cytarabine, palliative oral chemotherapy or best supportive care only, according to physician choice. The impact of geriatric scores on 6-months overall survival was analyzed.
Results: Between 2010 and 2015, 94 patients were enrolled, including 61.7% of males and 38.3% of females. Median age was 75.5 years (70-96). Initial median leucocytes, neutrophils, hemoglobin, and platelets counts were respectively 4.7 G/L (0.4-174), 1.3 G/L (0.1-5.4), 9.3 g/dL (5.3-13.2), 51 G/L (5-520). Median bone marrow blasts percentage was 55% (20-96). Cytogenetics was favorable, intermediate and adverse in 18%, 62% and 20% respectively. Intensive chemotherapy was chosen in 57.4% of patients, and low intensity or palliative approach in 42.6% of patients. Patients spent a median of 30.5 days in hospital (0-119), received a median of 12 (0-44) red blood cells units and 2 (0-33) platelets units. Global geriatric assessment of patients is reported in Table 1. By univariate analysis, prognostic factors associated with a reduced survival were high dementia risk (HR=3.63, 95% CI=1.4-9.3, p=0.004), high ECOG score (HR=2.1, 95% CI=1.1-4, p=0.02) and high risk of denutrition (HR=3.43, 95% CI=1.33-8.9, p=0.007), while intensive chemotherapy was associated with a better outcome (HR=0.45, 95% CI=0.2-0.9, p=0.014). Multivariate analysis identified high risk of denutrition as independently associated with reduced survival (HR=3.08, 95% CI=1.17-8.11, p=0.02). Intensive chemotherapy treatment tended to impact prognosis but was not statistically significant (HR=0.54, 95% CI=0.27-1.01, p=0.08).
Conclusions: In a prospective cohort of newly diagnosed AML elderly patients, an exhaustive standardized geriatric assessment at diagnosis identified high risk patients for mortality. The most relevant prognostic factor was nutritional status, which correlated with overall survival. Other geriatric scores and scales did not impact prognosis, which highlights the difficulty of global evaluation in this population. Patients treated with intensive chemotherapy tended to have a better outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal